Over the past decade, the U.S. healthcare system has worked on creating a streamlined digital record for patients and providers. Digitizing patient data has produced many benefits, including maintaining patient history, providing patients with access to their own data, and using that information to achieve accurate billing. What the healthcare industry lacks, though, is an operations platform for patient flow.
Having an automated digital care plan that connects patients throughout the care continuum, only engaging the care team when necessary, will revolutionize U.S. health care. The airline industry found success in the early days with their equivalent, the “flight plan.” This has evolved into a digital trip experience.
Passengers seamlessly interact with their flight journey through multiple channels, including websites, email, short message service (SMS), voice, and apps. Airlines report their real-time status and share automated updates about everything from availability, airport instructions, flight delays, and upgrade opportunities. Passengers move quickly through formalities and feel relaxed and in control of their trips.
As this travel information is integrated with baggage handling systems, airlines are equipped with real-time information about where a piece of baggage should be headed, allowing them to anticipate potential issues and operate transparently.
During boarding and takeoff, preflight checklists connected to central airline and airport IT systems provide flight crews with the most up-to-date policies, procedures, and alerts, while traffic control systems coordinate which planes can take off at which times.
All of this creates a productive, efficient, and seamless flight experience for all stakeholders, engaging all parties throughout the process to minimize cancellations and lost revenue.
Why can’t something like this exist for health care?
What Is Care Traffic Control?
The manual labor required to coordinate various stakeholders and procedures has historically held providers back. But, by automating protocols throughout the care plan, providers can pull relevant information from all necessary care teams and orchestrate operational processes in the background. This means tasks can be completed efficiently and on time, while expectations are managed to create a seamless care pathway.
Using the care traffic control approach, care teams manage by exception. Because care plans are digitized, automated, and orchestrated across teams and settings, the care team is efficiently tasked at the right time and at the right place while capitalizing on virtual patient engagement techniques as far as possible. The care team only intervenes with manual engagement when needed.
Taking advantage of investments in electronic health records (EHRs) plays a major role in this, as health records data inform care traffic control of patient status, missing gaps in care, and pathway compliance. However, providers lack a platform to operationalize the flow of care tasks that connect patients to care teams in an orchestrated journey.
Personalizing Pathways
Typically, care traffic control has three simple pathways: high-, medium-, and low-risk patients. High-risk patients—such as the elderly or individuals with comorbidities—are passed through a highly scrutinized pathway with frequent manual intervention, whereas low-risk patients may receive hands-off care such as automated engagement and digital coaching.
Patient preference is another way of looking at personalization. For instance, providers must effectively communicate with each patient in ways he or she prefers. This could mean text messages, phone calls, or even postal letters; if one strategy doesn’t work, detect and adapt it, and do so automatically.
Patient preference also plays into how providers target patient engagement initiatives. Tech-savvy patients who are willing to participate in data sharing will likely not require as much guidance along their care journey, while less engaged patients may prefer a manual approach—turning off the autopilot when the situation calls for it.
Care teams can even segment by compliance to a pathway. For example, if a patient hasn’t opened an email or completed an online form, this could indicate less compliance with certain parts of the pathway and, therefore, a high risk.
These analyses give providers the potential to become highly granular in personalizing their care delivery. Taking it a step further, anxiety questionnaires can pinpoint patients who are having second thoughts about an upcoming surgery. Meanwhile, personality and socio-demographic questionnaires can help adapt coaching instructions to the individual patient’s behavior.
Current and Future Benefits
In the same way that automation has improved the flying experience for passengers and airlines alike, it also pays off for patients, care teams, and profit margins. Providers not only see advantages in the short term, but they are also well-prepared for the future as alternative healthcare models focused on value-based care become widespread.
For example, implementing care traffic control helps coordinate pre-surgical readiness and identify risks that typically lead to delays. Late operating room (OR) cancellations are extremely costly, as a provider potentially leaves the OR vacant and teams scramble to reschedule patients.
Ambulatory surgery centers (ASCs) are often forced to let a canceled surgery slot go unfilled, with orthopedic surgery specifically seeing high cancellation rates. With average revenue at around $3,520 per procedure and ASCs doing approximately 6,000 procedures a year, this could amount to a loss of nearly $8.5 million per year.
Care traffic control also addresses problems with risk-based payment models. By deploying a platform for care delivery operations, providers can efficiently use the resources they already have, including their EHR, to deliver care consistently and, ultimately, protect themselves from margin erosion.
The positive impact of care traffic control is especially powerful when it pairs patients with enhanced recovery techniques, allowing patients to achieve an improved outcome quickly.
Specifically, improvements in patient education, transportation services, and clinic efficiency help engage patients in follow-up care.1 Researchers have found that, while nearly all patients recognize the importance of follow-up care, they still do not always attend their appointments, and this is an area where care traffic control plays an important role.
Finally, there is an emerging need in today’s market that’s being driven by the prevalence of smartphones, along with patients who want to take advantage of virtual care delivery and digital communication. Using care traffic control, providers can expand the reach of their services to low acuity and underserved populations. The beauty of this approach is it applies to a range of provider issues, from appointment reminders, to post-op check-ins via SMS, to avoiding readmissions.
All in all, automated care pathways help providers overcome hurdles that are all too common—from reducing appointment no-shows and increasing revenue through patient recall to reducing readmissions through deploying enhanced recovery techniques before surgery.
Care Traffic Control in Practice
In one example, Lumeon, Inc., a care pathway management company, is working with a well-known, large U.S. integrated delivery network that faced issues with high cost and low throughput in preparing patients for surgery. The network wanted to find a way to manage this, particularly by helping nurses handle their patients efficiently and in a standardized way.
The network is deploying the Lumeon platform and using its care pathway management capabilities to screen patients, assess patient risks, and digitize patient education and coaching. Additionally, the network’s care teams monitor patient readiness in real-time, avoiding the need to chase routine tasks. Digitizing and automating the entire patient experience also let patients know what to expect, which reduces anxiety and improves ongoing coaching.
It Won’t Happen Overnight
From pre-surgical readiness to discharge management, recovery, and follow-up, health care has the opportunity to digitize the patient pathway from A to Z and ensure that patients get the fastest possible recovery in the shortest possible time. Like the autopilot function in airplanes, care teams are always in control and can also “flip a switch” whenever required, while they focus on engaging those high-risk patients with complications who are most in need.
This is not an overnight process.
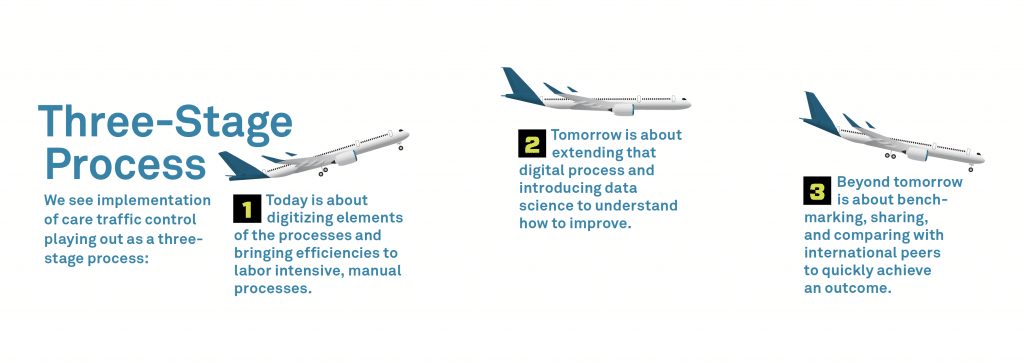
The single biggest barrier in health care is fear of change. Whenever we talk about pathways and processes, people are concerned that this may bring significant change to the ways they work. Therefore, the right approach is to introduce change gradually. Healthcare organizations need to ensure that they focus on a smooth, integrated process, using proper training methods and working with physicians and staff to avoid administrative issues (see “Three-Stage Process”).
Like the airline experience, it needs to be an end-to-end, branded provider experience that differentiates a provider beyond its competitors.
By digitizing the patient journey and care plan through the right automation platform, we control how and where we introduce change into the patient journey. The greatest care traffic control beneficiary is patients, who receive a new digital health experience that guides them in the right direction, toward a fast and improved recovery.
Reference
A.C. Thompson, M.O. Thompson, D.L. Young, et al. 2015. Barriers to Follow-Up and Strategies to Improve Adherence to Appointments for Care of Chronic Eye Diseases. Investigative Ophthalmology and Visual Science, 56(8). Accessed November 26, 2018 at iovs.arvojournals.org/article. aspx?articleid=2396444.

